Interventional Treatments
Interventional Treatments
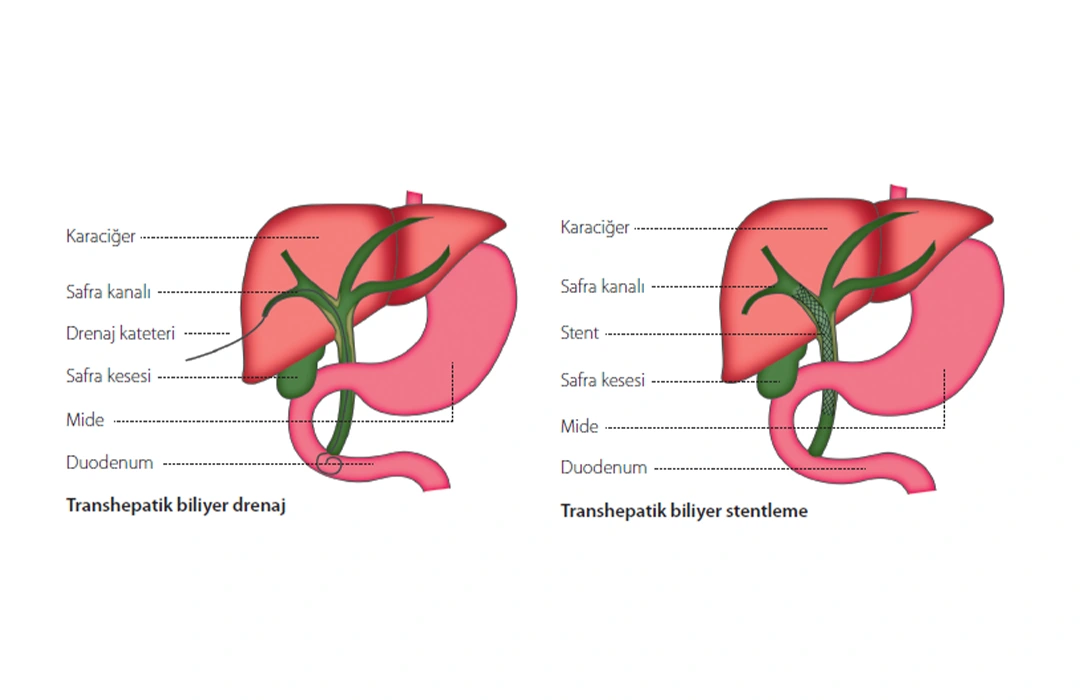
Percutaneous Transhepatic Biliary Drainage (PTBD) & Stent Placement
How is bile excreted from the body ?
The liver produces bile, which is necessary for digestion. It drains bile into the intestines through bile ducts. If these ducts become blocked due to conditions like stones or tumors, bile cannot flow into the intestines and accumulates in the liver, causing jaundice and itching throughout the body.
What is Percutaneous Transhepatic Biliary Drainage (PTBD) ?
Often referred to as PTK, this procedure involves placing a small plastic tube (catheter) through the abdominal skin into the liver’s bile ducts. This catheter drains bile from the liver into an external collection bag. In some cases, the catheter is advanced further to bypass the blockage, allowing bile to directly flow into the intestines. This treatment helps resolve jaundice by enabling the proper excretion of bile from the body.
What is Percutaneous Transhepatic Biliary Stent Placement ?
In suitable cases, a metal or plastic stent is placed through the catheter used in PTBD to keep narrowed or blocked bile ducts open. The stent helps bile flow into the intestines and prevents the development of jaundice. Stent placement is often performed after PTBD to remove the external drainage tube and bag. In some cases, the stent may be placed during the drainage procedure if the bile duct is not infected. The stent improves patient comfort but may not be appropriate for all patients.
How Will This Procedure Benefit Me ?
Biliary drainage reduces pressure on the liver, allowing it to function normally and lowering the risk of infections and liver failure. Jaundice symptoms (yellowing of the skin and eyes) will improve, and itching will decrease.
Biliary drainage may also be needed as preparation for other surgical interventions related to the bile ducts. Stent placement can provide long-term relief from bile duct blockages, ensuring bile flows into the intestines.
How Should I Prepare for the Procedure ?
Before the procedure, blood tests will be done to assess liver and kidney function and to check your clotting levels. You may need to stop or adjust the dosage of certain medications; consult with your doctor.
A contrast-enhanced CT or MRI scan of the liver is required if it has been done within the last month. You must also fast from the night before the procedure, and intravenous fluids may be provided.
How is Percutaneous Transhepatic Biliary Drainage (PTBD) Performed ?
The procedure is carried out in the hospital’s interventional radiology suite with the aid of angiography and ultrasound imaging. You will be connected to a monitor to track your oxygen levels, heart rate, and blood pressure. Sedatives and pain relief medications will be given.
The interventional radiologist will first use ultrasound and/or angiography to guide a needle and then a wire into one of the bile ducts. The procedure can be done through the skin on the right side of your abdomen, just below the chest. Once the wire is in place, small tubes will be inserted through it to form the pathway for the drainage tube. You may feel some pressure or discomfort during this procedure, but it will be painless due to local anesthetics and painkillers.
Once the drainage tube is positioned, it will be secured in place with stitches or adhesive bandages. A sterile dressing will be applied and changed regularly.
How is Percutaneous Transhepatic Biliary Stent Placement Performed ?
If a biliary drain is already in place, a guidewire is passed through the drain and advanced to the intestines. The existing drain is then removed, and a stent is placed. The interventional radiologist will ensure the stent is correctly positioned, after which the drain will be removed. If a drain is not in place, a similar procedure is followed to access the bile duct and place the stent.
Before or after stent placement, the narrowed bile duct may be widened using a special balloon, which can cause discomfort in the upper abdomen. This pain can be managed with strong pain relievers. After the procedure, adhesive bandages will be applied to the entry site.
What Are the Risks ?
There is a small risk of bleeding at the insertion site, or into the abdomen or bile ducts. If the tube is inserted through the ribs, you may experience some pain at the insertion site. The drain or stent could move or become dislodged. Over time, the stent could become blocked. There is also a risk of infection in the bile ducts. Bile could leak into the skin, abdomen, or the chest around the lungs. These issues should be reported to your doctor.
What Can Happen After the Procedure? What is the Follow-Up Plan ?
After the procedure, you will be moved to your hospital room for rest and monitoring. You may feel some pain in the insertion or upper abdominal area, as well as mild nausea, which can be treated with medication. You may also be prescribed antibiotics. If you have an external drain and collection bag, it is essential to follow proper care instructions and prevent dislodging. Nurses will monitor the bag and record the fluid amount.
Proper care of the biliary catheter is crucial. If you are discharged, ensure you receive detailed instructions about tube cleaning and dressing changes. Follow-up visits will include a plan for regular catheter or stent maintenance, including tube changes when necessary.